AR Recovery Services
Years of expertise have helped us build a framework for managing the AR processes. We use a streamlined strategy that is both quick and efficient.
Features of our AR Recovery Services
- Research Payer Medical Policies, Appeal Rights, Filing and Appeal Deadlines, Etc.
- Initial Denial/ Non-Payment Resolution
- 1st, 2nd, and 3rd Level Appeals
- Mass Appeals/ Mass Refiling of Claims as Required
- Filing of Secondary and Tertiary Claims as Required
- Patient Billing (When Applicable)
- Identification and Escalation of Obsolete AR to Client
- Denials Analysis and Management
- Root Cause Analysis
- Dedicated Account Management
- Weekly and Monthly Progress Updates
What Makes Us Unique
Hurricane Management provides a broad spectrum of AR healthcare receivables solutions and management services, including the recovery of lost revenue from accounts that have been outstanding for more than 120 days. Even from accounts that were supposed to be lost causes, our methodology has proved to be extraordinarily impactful at enhancing recoveries.
Unlike numerous different medical billing recovery businesses, Hurricane Management offers accounts receivable recovery services as a stand-alone option, rather than as part of a revenue cycle management package. We don’t believe in a one-size-fits-all solution to AR management and strive to tailor our solutions to your specific needs.

Methodical Evaluation
When one of our accounts receivable managers takes on a new client, the first thing they do is go over every unsettled claim and run an AR analysis. There may be some that have expired or are no longer collectible for various reasons, but we track down every single one that can be salvaged and get to work.
In the account receivable billing process, we’re not only hunting for the “easy targets”. Most AR collection businesses only look for high-dollar medical claims billing in aged accounts receivable, but we know how quickly lesser sums compound up for our clients, so we check every claim that could still be reimbursed.
Prioritization
Our AR analysis team monitors and follows up on outstanding claims on a regular basis to guarantee that none of them expire before we can process them. To be reimbursed, claims must be filed, processed, and submitted in a timely manner. We remain on top of each payer’s criteria with innovative analytical tools, allowing you to earn the most income possible. We follow up with each payer on a regular basis to collect past-due payments and improve your bottom line. Our accounts receivable management systems allow you to focus on your practice while guaranteeing that the unpaid amount is promptly and appropriately returned.

Claim Revision and Resubmission
Our committed taskforce doesn’t let a single claim get rejected, denied or underpaid. Our resources can even be employed to stay on top of your current claim denials and rejections. As a result, they can pinpoint the causes of problems and eradicate them from your revenue cycle management system permanently. After making the necessary modifications or refinements, we file an appeal with the insurance or government payers to have the payment reconsidered. This strategic approach will have a substantial beneficial influence on the financial stability of your practice. It becomes simpler for healthcare providers to get payments on time if we improve medical accounts receivable administration.
Patient Communication
If the AR team concludes that the patient is responsible for paying the outstanding balance, we create an easy-to-understand report and deliver it to them. We can also manage direct encounters with your patients if that is something you want us to undertake. Uncollected patient collections will never slow down your healthcare revenue cycle management with our dependable medical billing collection agency.
We’ve discovered that patients are considerably more likely to pay their bills if they understand the charges and agree on the amount owed, so we try to make everything as transparent as possible. If you want us to, we’ll even accept their calls and answer their inquiries.
AR Recovery Is One of Our Strengths
Every year, a significant amount of money is lost owing to improperly managed outstanding claims. We have a specialist recovery billing team with a high success rate in obtaining refunds for what other companies consider uncollectible. It’s common knowledge in the collections industry that the longer a bill remains unpaid, the less likely it is to be paid—but rather than abandoning old AR recoveries and bills, we’ve decided to take a different approach. Our account recovery services team interprets this as a signal to identify and investigate any outstanding claims immediately. Few medical AR billing providers will take on older accounts receivable recovery solutions, and if they do, they will charge a premium cost. Our approach makes the process more efficient, allowing us to work economically on old AR Recoveries and low-value claims. Some of the characteristics of our AR recovery system are as follows.
All Claims Pursued
Many billing businesses avoid small claims and those with a low chance of being paid, but not Hurricane Management. Due to the efficiency of our system, we may attempt to reimburse each claim.
Prioritization in the Interest of Maximum Recovery
We prioritize claims to ensure that none expire needlessly, and we use the most efficient technique to gather the largest potential recovery.
Dedicated AR Recovery Services Team
We allocate a specialized team of expert medical billers to focus on AR follow-ups in medical billing and researching every outstanding claim when we contract to assist with AR recovery.
Pay Only for Successful Reimbursement
Despite the fact that sorting through all of your outstanding claims is a lot of work for us, there is no chance of you losing money on old AR. We only charge a modest portion of the money recovered as fees. You do not pay us if we are unable to obtain money for a claim, therefore there is no risk to you.
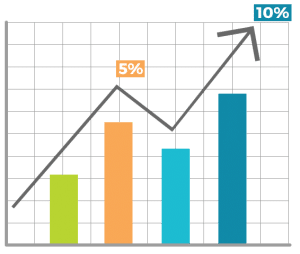
Collection Ratios Over 90%
Our accounts receivable collection services team has routinely recovered over 90% of claims dating back over a year. That kind of revenue may easily make a major impact in a medical practice's financial performance.
Appeal Rejections and Denials
The majority of claim rejections and denials are due to billing mistakes or omissions that our skilled billing staff can promptly remedy. With our accounts receivable management best practices, you can quickly identify and handle difficult situations.